Home > Milk supply, expressing & pumps
Milk supply, expressing & pumps
Your Milk Supply
In the first few days, it can feel like your baby is constantly feeding. Learning about the size of your baby’s stomach can help you understand how much and how often your baby needs to feed.
This photograph of marbles shows how small your baby’s stomach is in the first few days after being born. Because of the stomach being so small, your baby will need to feed often to keep himself feeling full. After a few days, he will be able to take in a little more milk with each feed but will still need to feed every 90 minutes to 2 hours.
How often should I feed my baby?
You might hear about getting your baby into a routine and giving feeds at certain times of the day and night. The good news is, if you let your baby set the pace for feeding in the early weeks, he’ll be happier because he won’t be kept waiting when he’s hungry. Crying increases the level of stress hormones in his body and by responding to his hunger, you will produce the right amount of breast milk for him. If you try to cut down breastfeeds, you may not make enough milk for your baby’s needs.
Keeping your baby close to you will help you to recognise the little signs they make, known as baby feeding cues, to tell you they are hungry. Recognising these cues is important because the sooner you respond to them, the less frustrated your child will be between feeds.
How long should each breastfeed last?
Every baby is different so how much milk a baby needs will vary and it’s best to be guided by your child. Your baby will let you know when they have drunk enough milk.
Your baby does not need drinks of water when breastfed so a baby who wants a thirst quenching drink and not a feed for hunger will just take a small amount of feed.
What are Prolactin and Oxytocin and why are they important for breastfeeding?
Prolactin
- Prolactin is a hormone made in the pituitary gland of the brain, it is the main hormone necessary for the production of breast milk. During pregnancy, prolactin prepares your breasts to make breast milk.
- The high levels of oestrogen and progesterone produced by the placenta, prevent the prolactin from making a large amount of mature breast milk.
- After your baby and the placenta leave your body, your oestrogen and progesterone levels go down which allows the prolactin to rise and signal to the milk-making glands in your breasts to make breast milk.
- In the first few days after the birth of your baby, prolactin is responsible for the tremendous surge in breast milk as your colostrum changes over to transitional breast milk.
After the birth of your baby, the initial increase in prolactin is what gets milk production started, but it’s not enough to maintain the production of breast milk. To keep making breast milk, you need to breastfeed or express. The best way to increase your prolactin levels is to breastfeed or express very frequently.
Oxytocin
- Oxytocin is a hormone produced by the pituitary gland in the brain. It has many functions in the human body. It increases relaxation, lowers stress and anxiety, lowers blood pressure, and causes muscle contractions.
- Oxytocin is also the hormone involved in social relationships, bonding, trust, and love and is known as the mothering hormone, the anti-stress hormone and the hormone of love
- During childbirth, oxytocin causes the uterus to contract and push out the baby.
- Breastfeeding stimulates the release of oxytocin from your brain. It allows your baby to get the breast milk from your breasts and it causes your uterus to shrink down after the birth of your baby.
- Oxytocin fosters love, nurturing, and a strong emotional bond between you and your child.
When your baby breastfeeds, or you express your breast milk, the nerves in your breasts send a signal to your brain to release the hormones oxytocin and prolactin.
The prolactin tells the milk glands in your breasts to make more breast milk, and the oxytocin is responsible for getting the breast milk from your breasts to your baby.
The Signs That Your Body is Releasing Oxytocin
How can you tell if the oxytocin in your body is doing what’s its suppose to do? Here are some of the signs you can look for:
- A tingling or a pins-and-needles sensation in your breasts.
- Cramping in your uterus when you breastfeed.
- Hearing your baby swallow while you’re breastfeeding.
- Breast milk is leaking from your breasts.
- Feeling happy and relaxed after you feed your baby.
Stress, tiredness and pain can interfere with the Release of Oxytocin
Stress, tiredness, illness, fear, embarrassment, alcohol and smoking can all affect the release of oxytocin, interfere with your let-down reflex, and keep your baby from getting the breast milk from your body.
- If you’re in pain following a caesarean section, or for any other reason, you should talk to your Doctor about pain medication. If you are experiencing pain whilst breastfeeding please get help and advice from your midwife, health visitor or infant feeding peer support worker
- The first two weeks of breastfeeding are critical. Most new mothers experience some baby blues which come with the extreme changes in hormones just after birth and with the beginning of breastfeeding. You can lessen the impact of the changes by arranging a support system. Let your friends and family help you if you need a break. Let them cook for you or watch the baby while you take a nap.
- You need rest and sleep. Your baby’s sleep patterns have a big impact on your own sleep. For your own physical and emotional health, it is important that you get the sleep your body needs to lessen the effects of hormone changes. Try to relax when breastfeeding and rest as much as you can, which may mean ignoring the housework!
- Keep your baby close to you and let the oxytocin and prolactin work to give you all of the calming and bonding help with your baby.
Breast Milk is amazing!
Your baby has had tastes of what you eat from the amniotic fluid it is in while in your womb. These tastes from the food you eat then continue as you breastfeed your baby and this is why breastfed babies usually wean onto food better. What you choose to eat and drink flavours your breast milk.
Your breast milk is unique, it alters throughout the day and is like a dose of medicine for your baby. Your milk will always be perfect for your baby.
During each breastfeed, your milk changes slightly,
- the beginning of a feed has a mix of more water
- as the feed progresses, the mix changes to less water and more fat.
- at the end of the feed, your baby is receiving fat rich milk and will come off the breast on his own
Every feed will be different though; think of your appetite – sometimes you might just need a snack and other days a three-course meal. In the same way, your child might only need a quick feed or a much longer one.
Will I produce enough milk?
Breastfeeding works on a supply and demand basis; simply put, the more you breastfeed your baby, the more milk you will produce. You will make plenty of milk if:
- your baby is positioned and attached to your breast properly
- you are feeding him when he asks for it
- you are not replacing breast milk with formula feeds (see the NHS Sheffield leaflet, Breastfed babies and formula milk
How do I know if my baby has had enough milk?
You will know when to stop breastfeeding because a baby who is well attached will stop feeding when he has had enough. He will usually push out the nipple – he may look sleepy or even drunk or he may be calm and look around. If he is still awake offer him the other breast. He may want some or none of it. Offer that breast first next time you feed. Another way to check whether your child is getting enough milk is the number of wet and dirty (soft, yellow poo) nappies he produces and how much weight they are putting on after the first week.
What is Cluster feeding?
It’s normal for young babies to need frequent feeds. Sometimes a baby will have several short feeds clustered together. Feeds will tend to get quicker and more spaced out as your child grows. A newborn child might need eight to 12 feeds a day or more. It’s impossible to over-feed a breastfed baby, so relax and let him guide you.
 Try not to give your baby other food or drink
Try not to give your baby other food or drink
The more mum’s milk you give your baby, the more milk you produce. Giving other food or drink will reduce your milk supply.
If you give your baby less mum’s milk, it will not protect your baby against illness as effectively.
Feeding your baby solid food before they are ready (at around 6 months) could lead to him or her getting an upset tummy.
The benefits of expressing breast milk:
- Expressing a little bit of colostrum (first milk) can encourage your baby to feed in the early days.
- An engorged breast is one that is overfull with milk. If you are engorged or uncomfortable you will probably need to express some milk to soften the breast to help baby gain a good attachment. After the baby has finished the feed if the breast still feels over-full it would be best to express it until it feels softer, lighter and more comfortable. Remember, the breast needs to be well drained.
- If you have a premature or ill baby which is unable to breastfeed. In this case, it is important to start expressing milk as soon as possible after birth.
- When you feel the time is right to return to work, or you choose to have a night out with friends for example, expressed milk can be used. Your baby’s carer can feed him while you are out, giving you a little more freedom whilst being safe in the knowledge that your baby is still receiving all of the goodness of your breast milk. Similarly, if you are separated for any reason, such as if your baby is ill and needs to be hospitalised, your expressed breast milk can continue to be used for feeds even when you are not there. See the section on how to give expressed milk to your baby.
When you feel the time is right to return to work, or you choose to have a night out with friends for example, expressed milk can be used. Your baby’s carer can feed him while you are out, giving you a little more freedom whilst being safe in the knowledge that your baby is still receiving all of the goodness of your breast milk. Similarly, if you are separated for any reason, such as if your baby is ill and needs to be hospitalised, your expressed breast milk can continue to be used for feeds even when you are not there.
It is not true that expressing an engorged breast increases the amount of breast milk – on the contrary if the milk is not drained it could lead to inflammation (‘mastitis’) and ultimately reduced milk production.
If you are still unsure about how to express your breast milk after reading the following pages, seek advice from your midwife, health visitor or a peer supporter – they will be happy to help you learn a way of expressing that’s right for you.
Expressing breast milk by hand
Always begin with clean hands and sterilised equipment – a wide-rimmed bowl is ideal.
It may take a few minutes to get the milk to flow. This is normal. It will help to warm the breasts using warm flannels and gently stimulate the breast by massaging.
Most women find it easier to express breast milk when their baby is nearby. Skin to skin contact with your baby naturally releases hormones that encourage your milk to flow. Failing this, if you can have a photograph of your baby, or something that smells like them close to you, this can also trigger let-down reflex and encourage lactation.
How to express by hand:
- Preparation – It is important to stimulate the breast by massaging, this helps the milk to flow. Spend a few minutes gently stroking the breast with the backs of your fingers or use light circular movements with your fingertips, all around the breast. Touching your nipple will also help.
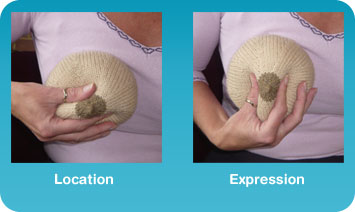
- Location – Place your finger and thumb about 2-3 cms away from the base of the nipple in a ‘C’ shape.
- Expression – Keeping your finger and thumb opposite each other, squeeze and release without moving the position of your fingers. It may take a few minutes for the milk to flow and it will start as drips. Collect the milk in a sterilised wide rimmed container. As flow slows down, rotate fingers around the breast and repeat the process to express milk from the whole breast. Repeat the process from step 1. on the other breast.
Expressing breast milk by pump
There are a number different breast pumps available, some manual, battery-powered or electric. Although expressing by pump can be quicker and less tiring than expressing by hand, it can be more uncomfortable, so try both methods and see what’s best for you.
Follow the manufacturer’s instructions on how to use your breast pump.
Always begin with clean hands and sterilised equipment.
You may find it difficult to get the milk to flow straight away. This is normal. It will help to stimulate milk flow by massaging your breasts or rolling the nipples as described in the preparation section above. It can also help to warm the breasts using warm flannels or by immersing them in warm water.
Storing breast milk
If you express breast milk to use at a later date, it is really important that you follow these steps:
- Sterilise all containers used to store the milk.
- Clearly mark each container with the date and time that the milk was expressed.
- Throw any unused milk away once it has been heated.
Guidelines for storage are:
- At room temperature for up to 6 hours (it must then be discarded if not used)
- Fridge (less than 4 degrees C): Up to 5 days at the back of the fridge (not the door)
- Freezer compartment of the fridge: 2 weeks
- Freezer (below 18 degrees C): 6 months
Defrost breast milk slowly in the fridge overnight and use within 12 hours. If needed quickly it can be thawed in a container of hot water. Once thawed, it should be used as soon as possible. Do not re-freeze milk after it has been defrosted.
You can add further cold expressed breast milk to the same bottle in the fridge after each feed that day, as long as the fridge is at 4 degrees C
How to give expressed breast milk to your baby
The most common way to give your baby expressed breast milk is in a bottle. It’s best to get your breastfeeding well established, however, before you try bottles. Some babies are happy to take a bottle from early on, and it doesn’t affect their ability to breastfeed. Others seem to be more easily put off by bottles.
The alternative is to use a special feeding cup or an egg cup for feeding expressed breast milk. These methods may be best for very new, ill or pre-term babies who have not yet learnt to feed from the breast effectively.
How to feed your baby with a cup
- Wrap your baby in a blanket so that he can’t move his arms, preventing him from knocking the feeding cup out of your hands.
- Use a special feeding cup, flexible little bowl or shot glass as a feeding cup
- Fill the baby feeding cup with about 1oz of pumped breast milk
- Position your baby upright so that he doesn’t choke. This is very important as baby may breathe in the milk causing it to go into his lungs.
- Put the rim of the feeding cup on baby’s lower lip and tilt it just enough for some of the milk to touch his lip. Usually baby will move his tongue down himself, to explore the cup.
- Allow your baby to lap the milk up himself, do not pour the milk into baby’s mouth.
- 30 minutes of cup feeding is usually sufficient especially in premature babies who may become tired quickly.
Tips for cup feeding a baby
- Baby cup feeding should be done during times when baby is alert.
- You might need to wind your baby a bit more often than usual with cup feeding.
- Keep a cloth or bib nearby to catch any spills or dribbles.
- Keep the cup on baby’s lips until he shows signs of being finished like moving his head away.
- NB – Don’t cup feed baby if you are able to breastfeed, especially not in the first few weeks while your milk supply is being built up.